What Makes a Complete Dental Implant System?
- by Shay ben shabat
What Makes a Complete Dental Implant System? Understanding Every Component for Reliability & Longevity
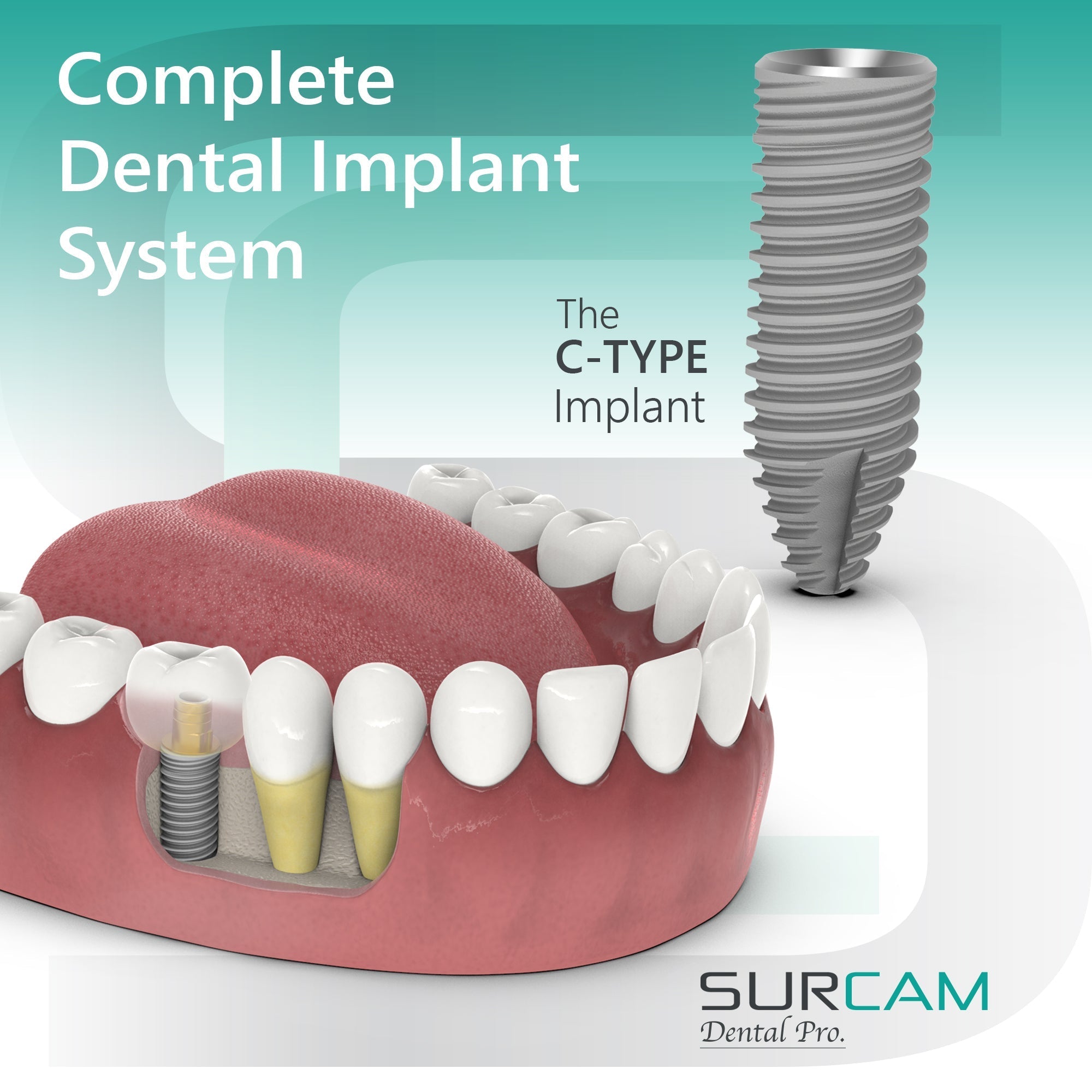
When evaluating implantology options, clinicians and distributors often focus on the implant itself. Yet what truly defines long-term success is the integrity of the entire dental implant system. A complete system brings together fixtures, abutments, prosthetic parts, and digital components in a way that ensures biological stability, mechanical strength, and clinical efficiency. When these elements align, dentists benefit from smoother workflows and patients experience healthier outcomes with fewer complications.
Behind every successful placement is a design that balances osseointegration, prosthetic precision, and soft-tissue preservation. That’s why understanding what makes up a system—and how each piece contributes—is essential when choosing between platforms such as internal hexagon and conical connection implants.
Core Components of Every Implant System
A modern dental implant system can be thought of as three essential layers, each supported by critical accessories:
-
Implant Fixture (the body or post): Usually manufactured from titanium or zirconia, the fixture anchors into bone. Its macro-geometry dictates primary stability, while its surface characteristics drive osseointegration.
-
Abutments: Acting as the bridge between fixture and prosthesis, abutments may be straight, angled, or custom. Their connection type—whether internal hexagon or conical—determines how loads are transferred, how well the interface seals against bacteria, and how stable the prosthetic will be over time.
-
Restorative Component: The visible part of treatment, ranging from single crowns to full-arch bridges or overdentures. Retention may be screw-based, cement-based, or supported by multi-unit frameworks, depending on the clinical scenario.
Supporting these three pillars are accessories that make the system complete: fixation screws that maintain preload, healing caps that shape soft tissue, transfers and analogs that replicate the implant in the lab, and digital tools like scan bodies and CAD/CAM Ti-bases that enable precision in modern workflows.
Key Insight: A dental implant is never just one component. Longevity and reliability come from the compatibility of every part across the system, ensuring each stage—from surgery to final prosthesis—functions seamlessly as one.

Additional System Elements & Accessories
A complete system anticipates the entire continuum of care—surgery, healing, impressioning, provisionalization, definitive prosthetics, and long‑term maintenance. The accessories below are not “nice to haves”; they are the control points that make outcomes reproducible.
Healing & Provisional Phase
Cover screws and healing caps protect the interface and contour peri‑implant soft tissue for a stable emergence profile. Selecting the right collar height to match tissue thickness reduces remodeling and streamlines your provisional timeline. Provisional components let you confirm occlusion and hygiene access without stressing the fixture.
Explore: Healing Caps – Internal Hex · Healing Caps – Conical Connection
Impressioning & Model Fidelity
Accurate models start with transfers that capture the 3D position and rotation of the implant, and analogs that replicate the connection in the cast or printed model. High‑tolerance transfers/analogs prevent marginal discrepancies at delivery and reduce remakes.
Explore: Transfers & Analogs – IH · Transfers & Analogs – CC
Multi‑Unit & Full‑Arch Foundations
For cross‑arch restorations, multi‑unit abutments create a leveled, screw‑retained platform that supports passivity and simplifies maintenance. Consistent cuff heights and available angulations help align trajectories and improve prosthetic access.
Explore: Screw‑Retained Multi‑Unit Abutments · Conical Multi‑Unit · Multi‑Unit System Trays (7 choices)
Digital Integration (Scan Bodies & Ti‑Bases)
Scan bodies translate intraoral position into precise CAD coordinates; CAD/CAM Ti‑bases provide a stable link between the designed prosthesis and the implant/abutment. Using connection‑specific libraries prevents rotational play and ensures a repeatable emergence profile.
Explore: Ti‑Bases – IH · Ti‑Bases – CC
Casting & Hybrid Workflows
When indications or lab preference call for it, casting abutments allow conventional workflows or hybrid analog‑digital approaches—useful for unique emergence needs or cost‑controlled cases.
Explore: Casting – IH · Casting – CC
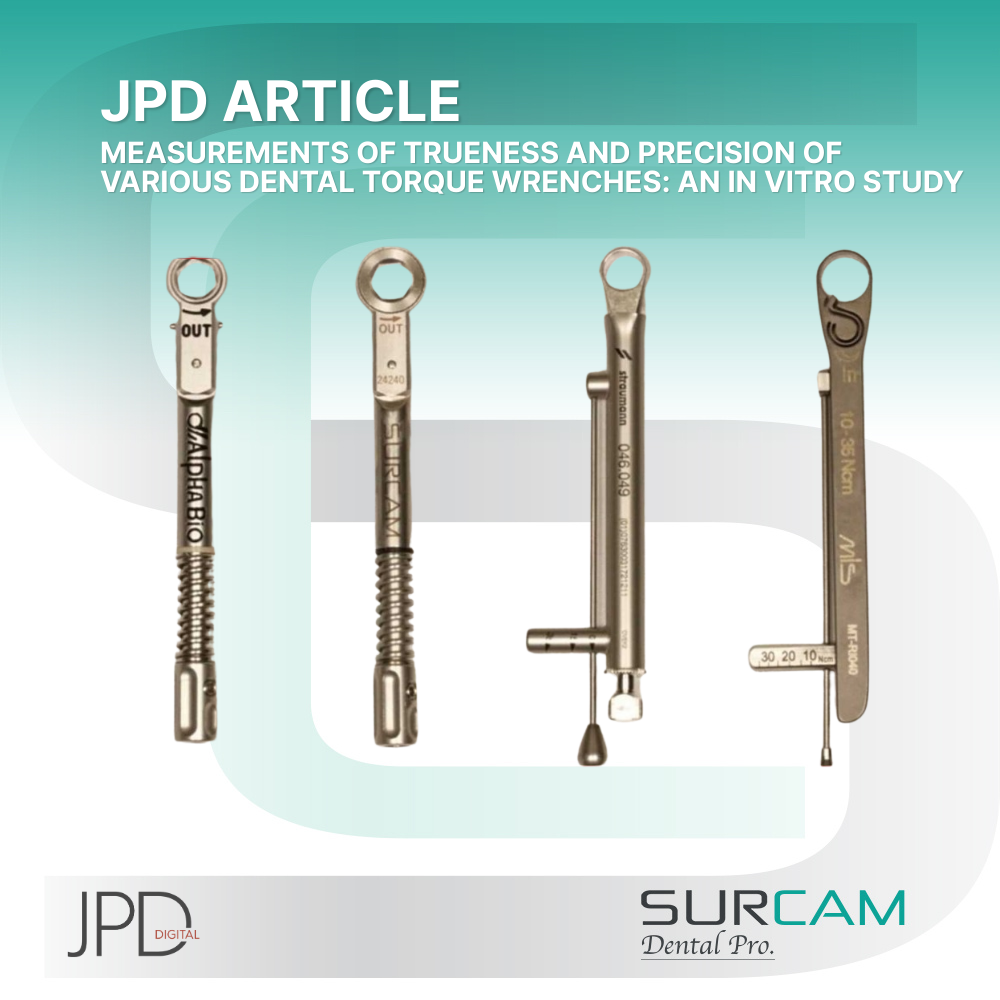
Instrumentation & Torque Control
Outcome stability depends on torque accuracy. Drivers, torque wrenches, and surgical tools help you achieve manufacturer‑specified preload and protect screws from over‑ or under‑tightening—key to minimizing loosening over time.
Explore: Tools & Wrenches
Bottom line: Systems that include purpose‑built accessories make each clinical step repeatable, reduce complication risk, and shorten chairtime for both routine and advanced cases.
Material & Surface Science
The reliability of any implant system depends not only on its geometry but also on the material composition and the surface technology that interacts with bone and soft tissue.
Titanium & Alloys
Commercially pure titanium and Grade 5 titanium alloy (Ti-6Al-4V) dominate implant manufacturing due to their balance of strength, biocompatibility, and corrosion resistance. Alloyed versions provide higher tensile strength, which is especially important for narrow-diameter implants.
Beyond bulk strength, the fatigue behavior of titanium alloys is critical in posterior and full‑arch cases. Grade 5 offers higher yield strength and better fatigue resistance than CP titanium, allowing slimmer components without compromising safety. Titanium’s natural oxide layer (TiO₂) provides corrosion resistance and promotes osseointegration; controlled anodizing can also aid visual identification (color‑coding) and influence surface energy for soft‑tissue friendliness on transmucosal parts. Proper machining tolerances and finishing (particularly on abutment cones and screw threads) reduce micromovement, protect preload, and improve long‑term stability.
Explore: Internal Hex Implants · Conical Connection Implants
Zirconia Options
Zirconia implants serve patients with metal sensitivities or demanding esthetic zones. Their one-piece designs reduce abutment connections, though long-term data is less extensive than for titanium.
Surface Treatments
Osseointegration is accelerated by surface modifications. Techniques such as sandblasting, acid etching, anodizing, or calcium phosphate coatings increase surface area and improve bone-to-implant contact. A roughened surface can shorten healing times and enhance long-term stability.
Bacterial Interaction
Surfaces are engineered not only to invite bone but also to discourage bacterial colonization. Hydrophilic treatments, combined with precise platform switching, can reduce inflammatory risk at the crestal bone.
In transmucosal and prosthetic regions, PVD titanium nitride (TiN) coatings offer practical advantages: increased surface hardness and wear resistance, lower plaque adhesion compared with untreated titanium, and a stable, biocompatible interface that helps maintain torque values over time. TiN’s warm gold hue can also improve esthetics under thin soft tissue. We apply TiN on our Prime Series multi‑unit abutments to enhance hygiene and durability in high‑load restorations.
Explore: Prime Series Screw‑Retained Multi‑Unit Abutments (TiN)
Clinical takeaway: Selecting systems with documented anti‑wear and anti‑plaque surface technologies (e.g., TiN on transmucosal components) can meaningfully reduce maintenance visits and protect peri‑implant tissues, especially in full‑arch protocols.
Implant–Abutment Interface Design
The connection between implant and abutment is the mechanical and biological seal that dictates long‑term stability. It determines how occlusal loads are distributed, how well micro‑gaps are controlled, and how resistant the system is to bacterial leakage.
Internal Hexagon
The internal hexagon, a six‑sided recess, remains one of the most widely used interfaces. It is easy to restore, broadly compatible, and cost‑efficient. However, its flat‑on‑flat geometry concentrates stress at the crestal bone and is more susceptible to micromovement and screw loosening.
Explore: Internal Hex Implants & Components
Conical Connection
The conical, or Morse taper, interface uses a wedged fit to create a friction lock between implant and abutment. This design minimizes micromovement, offers a tighter bacterial seal, and distributes forces deeper into the implant body—protecting crestal bone.
Explore: Conical Connection Implants & Components
Why the Interface Matters
-
Load distribution: Flat connections focus stress at the crest; conical designs spread it apically.
-
Bacterial control: Tapered interfaces reduce the “pump effect” and minimize peri‑implantitis risk.
-
Prosthetic reliability: Stable interfaces reduce screw loosening and fracture rates, especially under high loads or in full‑arch cases.
Clinical takeaway: While both designs achieve survival rates above 95%, conical connections consistently demonstrate superior bone preservation and fewer prosthetic complications—making them the preferred choice for demanding restorations.
Biological & Mechanical Criteria for Systems
A complete implant system succeeds only when it addresses both biological integration and mechanical reliability. The interplay of these factors determines long-term survival and complication rates.
Osseointegration Prerequisites
Primary stability is influenced by implant macro-geometry (taper, thread design, diameter) and surface topography. Roughened and treated surfaces accelerate bone apposition, while platform switching protects the crestal bone during remodeling.
Mechanical Load & Stress Distribution
The system must transfer occlusal forces efficiently. Narrow implants and flat connections place more stress at the crestal bone, while wider diameters and conical connections distribute load more evenly into the implant body and surrounding bone. This reduces marginal bone loss and screw complications.
Soft-Tissue Integration
Healing caps, emergence profiles, and transmucosal abutment finishes all shape peri-implant tissue stability. Surfaces such as titanium nitride (TiN) coatings can lower plaque retention and improve mucosal health, especially critical in full-arch prosthetics.
Explore: Healing Caps – IH · Healing Caps – CC
Clinical Balance
-
Biological success = osseointegration + soft tissue stability.
-
Mechanical success = resistance to micromovement, preload maintenance, and fatigue strength.
-
Systemic success = both dimensions working together, with parts engineered to function as one ecosystem.
Clinical takeaway: Choosing a system is not just about fixture design. It is about how every element—from surface science to connection geometry—works together to secure bone, protect soft tissue, and withstand years of functional load.
Lab / Digital Integration & Prosthetic Workflow
A system is only as reliable as its ability to integrate into both the surgical chairside process and the laboratory or digital workflow. Complete implant systems anticipate this continuum and provide tools that simplify communication between clinic and lab.
Transfers & Analogs
Traditional workflows rely on transfers to capture the implant’s position and analogs to replicate it in a model. High‑precision components ensure casts mirror intraoral conditions, reducing the risk of misfit and remakes.
Explore: Transfers & Analogs – IH · Transfers & Analogs – CC
Digital Capture & Design
Modern CAD/CAM workflows use scan bodies to translate intraoral implant position into digital data. Paired with Ti‑bases, they create a foundation for customized abutments, crowns, and bridges. Brand‑specific libraries maintain rotational accuracy and secure prosthetic fit.
Explore: Ti‑Bases – IH · Ti‑Bases – CC
Multi‑Unit & Full‑Arch Restorations
For cross‑arch or hybrid cases, multi‑unit abutments streamline screw‑retained prosthetics. Their role in both analog and digital workflows is critical—providing predictable seating, retrievability, and passive fit in complex restorations.
Explore: Multi‑Unit Abutments
Hybrid Workflows
Many labs now combine conventional steps (casting abutments, wax‑ups) with digital design. Systems that supply both analog and digital accessories give clinicians flexibility to adapt to each case without compromising accuracy.
Clinical takeaway: Complete implant systems deliver not just fixtures and abutments but a workflow ecosystem—ensuring seamless translation from intraoral placement to laboratory fabrication and final prosthesis delivery.
Regulatory, Certification & Quality Assurance
Beyond design and workflow, a complete implant system must be verifiably safe and compliant. Regulatory approval ensures materials and manufacturing meet strict international standards.
Global Standards
Systems are evaluated under ISO quality management and biocompatibility testing protocols. Compliance with FDA clearance in the United States and CE marking in Europe confirms that implants, abutments, and accessories are safe for clinical use.
Sterility & Packaging
Each sterile-packaged implant and component undergoes validated sterilization procedures (gamma irradiation, ethylene oxide, or equivalent) and is sealed to maintain integrity until surgery. Lot numbers allow for full traceability from manufacturer to patient record.
Material & Process Verification
Mechanical properties (tensile strength, fatigue resistance) and surface characteristics are tested to confirm performance. This includes coating adhesion tests for treated surfaces like titanium nitride.
Why This Matters for Clinics & Distributors
Clinics need confidence that their implant supplier adheres to globally recognized standards. Distributors gain trust when product lines can demonstrate consistent certification and verifiable traceability across every SKU.
Explore certified systems: Internal Hex Collections · Conical Connection Collections
Clinical takeaway: A true implant system is defined not just by engineering but by documented quality assurance and regulatory compliance, ensuring patient safety and long-term reliability.
Case Example: Full‑Arch System vs. Single Tooth System
Looking at implant systems in context shows why completeness matters. A single‑tooth case and a full‑arch restoration demand very different accessory sets, yet both rely on a system’s internal consistency.
Single Tooth Replacement
A straightforward single implant requires the fixture, abutment, and restoration—plus healing caps and impression tools. With reliable connections, tissue‑friendly surfaces, and accurate lab analogs, even simple cases benefit from a well‑engineered system.
Relevant collections: Internal Hex Dental Implants · Cemented Abutments – IH
Full‑Arch Rehabilitation
A complete arch supported by implants magnifies every detail. Beyond fixtures and abutments, the case requires multi‑unit abutments, torque‑controlled screws, surgical guides, CAD/CAM Ti‑bases, and prosthetic bars or frameworks. The quality of each accessory impacts passivity, hygiene, and long‑term stability.
Relevant collections: Conical Connection Multi‑Unit · Prime Series Multi‑Units (TiN) · CAD/CAM Ti‑Bases – CC
Lessons from Contrast
-
Single tooth: Simplified workflows, lower cost, high esthetic demand.
-
Full arch: Complex prosthetics, higher loads, accessory‑dependent success.
Clinical takeaway: The difference between a basic and a complex case underscores why a “complete system” is more than a fixture. Systems that provide the full accessory ecosystem give clinicians confidence from the simplest crown to the most demanding full‑arch restoration.
How to Assess Implant Systems Before Purchasing
With dozens of implant platforms available, it is easy to focus on fixture shape or price. Yet true value lies in how complete and supportive the system is over years of clinical use. A structured evaluation helps dentists, DMD‑run clinics, and distributors avoid costly gaps.
1. Material & Surface Verification
Confirm whether implants are made from Grade 4 CP titanium, Grade 5 Ti‑6Al‑4V alloy, or zirconia. Ask for documentation on surface treatments such as SLA, anodizing, or PVD TiN coatings and review corresponding test data for roughness, contact angle, and coating adhesion.
Explore: Internal Hex Implants · Conical Connection Implants
2. Connection Type & Prosthetic Ecosystem
A reliable system must provide both the implant–abutment interface (IH or CC) and the full prosthetic stack: healing caps, transfers, analogs, abutments, multi‑units, Ti‑bases, and screws. Availability of angled abutments and multiple cuff heights is crucial for tissue management and restorative flexibility.
Explore: Internal Hex Abutments · Conical Abutments
3. Digital Compatibility
Digital workflows are now standard. Verify that the system supports CAD/CAM libraries, scan body precision, and rotational accuracy of Ti‑bases. Systems lacking robust digital integration often create hidden costs in lab remakes.
Explore: Ti‑Bases IH · Ti‑Bases CC
4. Accessory Completeness
A complete ecosystem includes transfers, analogs, healing caps, casting abutments, and torque tools. For full‑arch protocols, ensure access to multi‑unit kits, prosthetic screws, and trays.
Explore: Transfers & Analogs · Casting Abutments · Tools & Wrenches
5. Mechanical Specs & Torque Data
Compare screw alloy, coatings, and manufacturer‑recommended torque values. Request fatigue testing and preload retention studies, particularly for narrow‑diameter implants and angled multi‑unit prosthetics.
6. Certification, Traceability & Warranty
Look for FDA clearance, CE marking, ISO certification, and clear lot traceability. Confirm sterilization methods, packaging integrity, and warranty terms on both implants and prosthetic components.
7. Logistics, Training & Support
Practical reliability extends beyond the operatory. Check stock availability, delivery times, and emergency replacement policies. Evaluate whether the supplier provides clinical education, lab training, and chairside support.
Clinical takeaway: Selecting an implant supplier is not only about fixture geometry or price. The right choice delivers a certified, digitally integrated, and accessory‑complete ecosystem that reduces complications, safeguards patient outcomes, and supports clinics with long‑term consistency.
FAQs (Frequently Asked Questions)
What are the three main parts of a dental implant system?
Every complete system includes the implant fixture (body), the abutment (connector), and the prosthetic restoration (crown, bridge, or denture). Supporting parts like screws, healing caps, and digital accessories complete the ecosystem.
Why do surface treatments matter?
Surface modifications such as SLA roughening, anodizing, or TiN coatings improve osseointegration, reduce bacterial colonization, and protect soft-tissue health over time.
How important is the implant–abutment interface?
The connection dictates load transfer, sealing ability, and long-term bone preservation. Conical connections generally offer superior stability compared to flat internal hex designs.
Are cheaper implant systems reliable?
Lower-cost systems may lack complete accessory ranges or digital support. While survival rates can be acceptable, missing components often create workflow challenges and higher long-term costs.
Do digital tools really make a difference?
Yes. Scan bodies, Ti-bases, and CAD/CAM libraries ensure restorations fit precisely, reduce remakes, and support guided surgery for safer placement.
Can one system serve both single-tooth and full-arch cases?
Only if it provides a full portfolio. Systems with multi-units, torque tools, and verified CAD/CAM support can scale from simple to complex restorations.
FAQs: Complete Dental Implant Systems
What are the essential parts of a complete implant system?
A reliable system includes the implant fixture, abutment, and restoration—supported by healing caps, transfers, analogs, screws, scan bodies, CAD/CAM Ti‑bases, and, for full‑arch cases, multi‑unit abutments.
Why does the implant–abutment connection matter?
Connection geometry (internal hex or conical) dictates load transfer, micromovement control, and the quality of the bacterial seal—all of which influence crestal bone stability and maintenance.
How do material and surface treatments affect outcomes?
Titanium grades and surface technologies (SLA, anodizing, PVD TiN) impact osseointegration, wear resistance, and plaque adhesion, shaping both healing speed and long‑term hygiene.
What should clinics check for digital compatibility?
Up‑to‑date CAD/CAM libraries, precise scan bodies, and Ti‑bases with reliable rotational indexing; these elements reduce remakes and improve prosthetic fit.
When are multi‑unit abutments necessary?
In cross‑arch and high‑load prosthetics, multi‑units create a leveled, screw‑retained platform that supports passivity, retrievability, and hygiene.
How important are certification and traceability?
FDA/CE/ISO compliance, sterile packaging, and lot numbers ensure device safety and accountability from manufacturer to patient record.
Do coatings like TiN really help?
Yes. PVD TiN on transmucosal and prosthetic components increases hardness, improves wear resistance, and reduces plaque adhesion—useful in full‑arch and high‑load scenarios.
What drives total cost of ownership?
Beyond the fixture price, reliability depends on accessory completeness, digital integration, torque stability, and support—factors that reduce remakes and emergency visits.
Conclusion
A complete dental implant system is defined not by a single fixture but by the integration of materials, connection design, surface science, digital tools, and accessory support. From single‑tooth restorations to full‑arch rehabilitations, the systems that perform best are those that maintain biological stability, mechanical reliability, and workflow consistency.
For dentists, DMD‑run clinics, and distributors, the choice comes down to partnering with a supplier that delivers a certified, fully integrated ecosystem. This ensures fewer complications, greater efficiency, and predictable patient outcomes.
👉 Explore Surcam Dental’s full line of Internal Hex Systems and Conical Connection Systems to match the right solution to every clinical scenario.
- Posted in:
- Educational